EU-Atlas: Dementia & Migration
| Largest group | 2. largest group | 3. largest group | 4. largest group | 5. largest group | |
| Absolute numbers | |||||
| PwMD per 100,000 inhabitants 65+ |
| Absolute numbers | PwMD per 100,000 inhabitants 65+ | |
| Largest group | ||
| 2. largest group | ||
| 3. largest group | ||
| 4. largest group | ||
| 5. largest group |
| Prevalence per 100,000 inhabitants 65+*, calculated by country of residence | |||
|---|---|---|---|
| high > PwMD |
minor > - PwMD |
||
| increased > - PwMD |
low ≤ PwMD | ||
| medium > - PwMD |
|||
| PwMD = People with a Migration background with Dementia *Bulgarien, Litauen, Malta, Polen in der Bevölkerung 60+ |
|||
| Absolute number of PwMD 65+ | |
| PwMD per 100,000 inhabitants 65+ |
United Kingdom
The UK has a long history of migration. Emigration and immigration took place due to various reasons such as British colonialism1,2, adoption of new policies2, work1,2, or the implementation of the 'Highly Skilled Migrant Program3. Between 1990 and 2019, the migrant population (born abroad) and the proportion of migrants in the total population more than doubled (3.7 to 9.6 million; 6.4 to 14.1%)4.
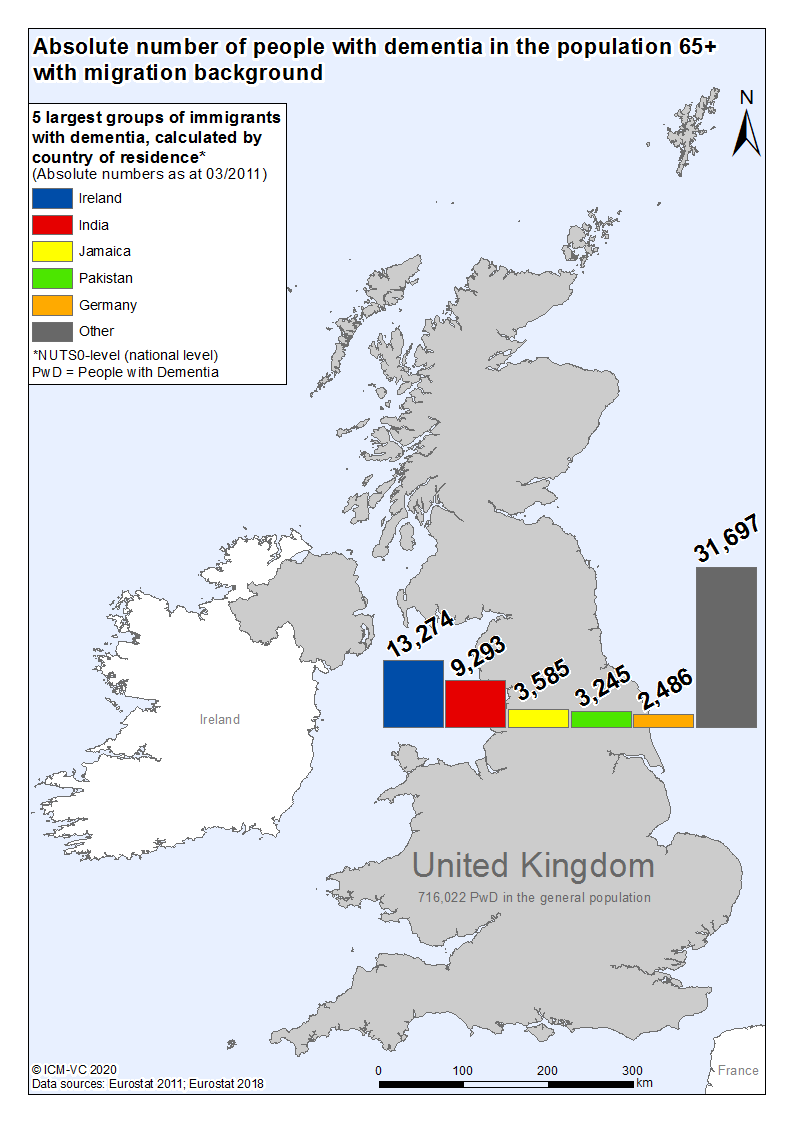
There are 10,500 PwM being 65 years or older. Of those, approx. 63,600 are estimated to exhibit some form of dementia. Calculations show the most affected migrant groups are presumably originating from Ireland (approx. 13,300), India (approx. 9,300), Jamaica (approx. 3,600), Pakistan (approx. 3,300), and Germany (approx. 2,500)5.
In the UK, six national dementia plans were identified (three in Scotland, one each in England, Northern Ireland, and Wales). Three further national documents on dementia care were also considered (two from England and one from Northern Ireland). Seven of these nine documents (three from England, two from Scotland, and one each from Northern Ireland and Wales) address migration to varying degrees6-14. According to contacted experts, three guidelines on care, treatment, and/or support for people with dementia are used in the UK (one each for England and Wales, Northern Ireland, and Scotland). All three guidelines refer to the topic of migration to varying degrees (two briefly, one in detail)15-17.
England's healthcare strategy is an integrative one where there is an effort to make ‘mainstream healthcare services’ more acceptable and fitting for minority groups. This is rather done than setting up specialised services for specific groups, although these also exist. Therefore, services for inpatient and outpatient care for people with dementia are nationwide available for migrants. Additionally, there are organisations providing culturally specific information on dementia. Still, existing care services for people with dementia are not fitting for migrants. Measures to provide intercultural care are locally in development.
Culturally sensitive care is part of healthcare professionals’ qualification nationwide. There are published professional standards for nurses and care workers and they specify what competence criteria are required for people to practice in dementia or old age care and they outline what is needed to provide a holistic, person-centred as well as culturally sensitive care. The proportion of professional caregivers with a migration background in inpatient and outpatient care is high in big cities. Due to low qualification and education, cultural needs in care are not being met.
Family, religious communities, migrant organisations, as well as inpatient and outpatient care services, are very important in supporting family caregivers of migrants with dementia. There are major differences in the suitability and utilisation of existing services by family caregivers of migrants with dementia and non-migrants with dementia. Accordingly, there is a very high need for specialised services providing support and information in England.
References
- Potnuru B, Sam V: India–EU engagement and international migration: Historical perspectives, future challenges, and policy imperatives. IIMB Management Review 2015, 69.
- Spafford M: 20th & 21st cntury migrations: 1900-2000s. [https://www.ourmigrationstory.org.uk/oms/by-era/1900%E2%80%932000]. Accessed 20 Jul 2020.
- Hansen R: Focus Migration: United Kingdom. In., vol. 12: Bundeszentrale für politische Bildung, Netzwerk Migration in Europa, Hamburgisches WeltWirtschaftsInstitut; 2007.
- International Organisation for Migration: International migrant stock as percentage of the total population at mid-year 2019; 2019.
- Eurostat: Census 2011; 2011.
- Department of Health: living well with dementia: a National Dementia Strategy. In. London: Department of Health of England; 2009.
- All-Party Parliamentary Group on Dementia: building on the National Dementia Strategy: change, progress and priorities. In.: All-Party Parliamentary Group on Dementia; 2014.
- Dementia Policy Team: Prime Minister’s Challenge on Dementia 2020: Implementation Plan. In.: Department of Health; 2016.
- Department of Health Social Services and Public Safety of Northern Ireland: improving Dementia Services in Northern Ireland: a Regional Strategy. In.: Department of Health, Social Services and Public Safety of Northern Ireland 2011.
- Health & Social Care Board of Northern Ireland: the Dementia Learning and Development Framework. In. Belfast: Health & Social Care Board of Northern Ireland; 2016.
- The Scottish Government Mental Health Division: Scotland's National Dementia Strategy. In. Edinburgh: The Scottish Government, Mental Health Division; 2010.
- The Scottish Government MHD: Scotland’s National Dementia Strategy: 2013-16. In.: The Scottish Government, Mental Health Division; 2013.
- Scottish Government: Scotland’s national dementia strategy 2017-2020. In. Edinburgh: Scottish Government; 2017.
- Llywodraeth Cymru Welsh Government: Dementia Action Plan for Wales 2018-2022. In.: Llywodraeth Cymru Welsh Government; 2018.
- National Institute for Health and Care Excellence: Dementia: Assessment, management and support for people living with dementia and their carers. In. Edited by National Institute for Health and Care Excellence, 97 edn. London: National Institute for Health and Care Excellence; 2018.
- National Collaborating Center for Mental Health: Dementia: A NICE–SCIE Guideline on supporting people with dementia and their carers in health and social care. Leicester UK: The British Psychological Society and Gaskell; 2007.
- The Mental Welfare Commission for Scotland: Standards of Care for Dementia in Scotland: Action to support the change programme, Scotland’s National Dementia Strategy: Scottish Government; 2011.

![[Translate to Englisch:] Logo RBS [Translate to Englisch:] Logo RBS](/fileadmin/_processed_/9/7/csm_RBS_Logo_RGB_0e245a98a4.jpeg)